National Leprosy Eradication Programme
NATIONAL LEPROSY ERADICATION PROGRAMME
Background: National Leprosy Control Programme (NLCP) was launched by the Govt. of India in 1954- 55. Multi Drug Therapy (MDT) came into wide use from 1982, and the National Leprosy Eradication Programme was introduced in 1983. The strategy of NLEP was based on controlling the disease through reduction in the quantum of infection in the population and reduction in infective source, thus breaking the chain of disease transmission. The programme was initially taken up in endemic districts and was extended to all districts in the country from 1993-94 with World Bank Assistant. Four Research & Training Institutes were established directly under DGHS, namely Central Leprosy Training and Research Institute Institutes (CLTRI) Chengalpattu, Regional Leprosy Training and Research Institute (RLTRI) at Raipur, Gauripur and Aska. In addition, a Training Centre was established at Agra under ICMR. Remarkable progress has been achieved in reducing the disease burden in the country.
India achieved the goal set by the National Health Policy, 2002 of elimination of leprosy as a public health problem, defined as less than 1 case per 10,000 population, at the National level in December 2005.
VISION:
“Leprosy-free India” is the vision of the NLEP.
Mission:
The NLEP’s mission is to provide quality leprosy services free of cost to all sections of the population, with easy accessibility, through the integrated healthcare system, including care for disability after cure of the disease.
Objectives:
a) To reduce Prevalence rate less than 1/10,000 population at sub national and district level.
b) To reduce Grade II disability % < 1 among new cases at National level
c) To reduce Grade II disability cases < 1 case per million population at National level.
d) Zero disabilities among new Child cases.
e) Zero stigma and discrimination against persons affected by leprosy.
Strategy:
To achieve the aforementioned objectives, the main strategies to be followed are:
1) Integrated anti-leprosy services through General Health Care system.
2) Early detection and complete treatment of new leprosy cases.
3) Carrying out household contact survey for early detection of cases.
4) Involvement of Accredited Social Health Activist (ASHA) in the detection and completion of treatment of Leprosy cases on time.
5) Strengthening of Disability Prevention and Medical Rehabilitation (DPMR) services.
6) Information, Education and Communication (IEC) activities in the community to improve self-reporting to Primary Health Centre (PHC) and reduction of stigma.
7) Intensive monitoring and supervision at Health and Wellness Centers and Block Primary Health Centre/Community Health Centre.
Following are the programme components:
o Case Detection and Management
o Disability Prevention and Medical Rehabilitation (DPMR).
o Information, Education and Communication (IEC) including Behaviour Change Communication (BCC)
o Human Resource and Capacity building
o Programme Management
Salient features of the National Leprosy Eradication Programme are:
1. Leprosy Eradication programme is a centrally sponsored scheme of Government of India.
2. NLEP functions under the umbrella of National Health Mission (NHM).
3. NLEP follows decentralized health planning and funds are sent to the states through State Health Societies.
4. Quality of services and sustainability is the main focus.
5. Disability Prevention & Medical Rehabilitation (DPMR) is a priority
6. Removal of stigma and discrimination is a part of the strategy.
Epidemiological Trends of important NLEP indicators from 1998 to 2020:
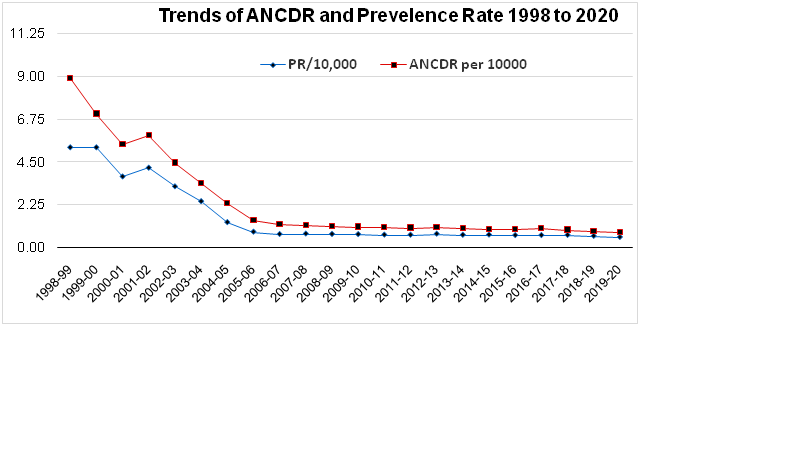
.png)
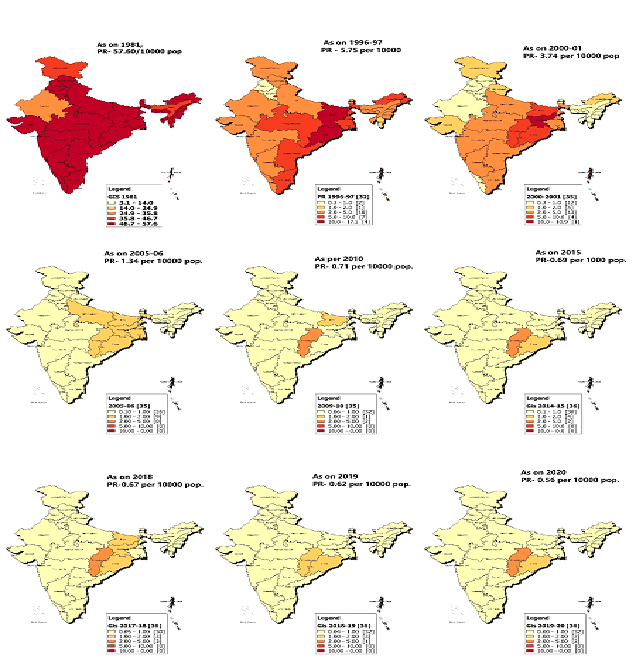
Various leprosy endemicity maps from 1981 to 2020, showing the prevalence of leprosy at different points of time, which evidently show that the burden of leprosy is shrinking in India.
Milestones of NLEP:
|
1948
|
Hind Kusht Nivaran Sangh
|
|
1955
|
National Leprosy Control Programme
|
|
1970
|
Definite cure in form of MDT was identified
|
|
1982
|
WHO - study group recommended use of MDT
|
|
1983
|
National Leprosy Eradication Programme, MDT started
|
|
1991
|
World Health Assembly resolution to eradicate leprosy by 2000AD
|
|
1993
|
World Bank supports the MDT programme phase -NLEP1
|
|
1997
|
Midterm appraisal of NLEP
|
|
1998-2004
|
Modified Leprosy Elimination Campaign
|
|
2001-2004
|
NLEP Project Phase II
|
|
2002
|
Simplified Information system Introduced
|
|
2005
|
Nationwide Evaluation of Project II
|
|
2005, Dec
|
Prevalence Rate of leprosy dropped to 0.95 /10000 population, and India achieved elimination status Nationally
|
|
2005
|
After Elimination, NLEP vertically run programme services integrated with General Health Care System under newly launched National Rural Health Mission
|
|
2007
|
Disability Prevention & Medical Rehabilitation Guidelines introduced for preventing disabilities at primary, secondary, and tertiary level
|
|
2007 – 2012
|
XI Five Year Plan advocated inclusion of Persons Affected with leprosy in all decision making exercise
|
|
2012
|
XII Five Year Plan adopted the Special Leprosy Action Plan for 209 High endemic districts in 16 States/UTs
|
|
2014
|
Independent Evaluation of NLEP by World Health Organisation
|
|
2014
|
Upgraded Simplified Information system implementation
|
|
2016
|
Rights of Persons with Disabilities Act, 2016
|
|
2017- 2019
|
New Initiatives
· Active Case Detections Campaigns (14 days) in high endemic districts
· Focused Leprosy Campaign (FLC) in low endemic districts
· ASHA Based Surveillance for Leprosy Suspects (ABSULS)
· Grade II Disability Epidemiological Investigation
· Implementation of Post Exposure Prophylaxis (administration of Single Dose of Rifampicin)
· Sparsh Leprosy Awareness Campaigns
· Introduction of NIKUSTH - A real time leprosy reporting software across India
|
|
2019
|
· External Evaluation of NLEP by World Health Organisation
· Convergence of leprosy screening with Comprehensive Primary Health Care programme of Ayushman Bharat, to screen 30+ years population at HWCs
· Convergence of leprosy screening with Rashtriya Bal Swasthya Karyakram (RBSK) to screen children (0-18 years) at Anganwadi Centers and Govt. schools,
|
|
2020
|
· Active Case Detection and Regular Surveillance (ACD&RS) guidelines rolledout.
· Convergence of NLEP with Rashtriya Kishore Swasthya Karyakaram (RKSK) for counselling the children of teen age group (13-19 yrs) about leprosy at Adolescent Friendly Clinics
|
Activities under NLEP:
- Diagnosis and treatment of leprosy- Free of cost Services for diagnosis and treatment (Multi drug therapy) are provided by all public health care facilities like primary health centres,govt. dispensaries, CHC, DH and Medical colleges throughout the country . Difficult to diagnose, complicated cases, reaction cases and G2D cases requiring reconstructive surgery are referred to district hospital for further management. All drugs, diagnostics and surgical /non surgical intervenytions are provided free of cost to all patients of leprosy across the board.
- Capacity building- Training of general health staff like Medical Officer, health workers, health supervisors, laboratory technicians and ASHAs are conducted every year to develop adequate skills for diagnosis and management of leprosy cases.
- IEC and counselling - Intensive IEC activities are conducted to generate awareness which will help in reduction of stigma and discrimination associated with persons affected with leprosy. These activities are carried through mass media, outdoor media, rural media and advocacy meetings. Major focus is also given on inter personnel communication.
- Disability Prevention and Medical Rehabilitation –For prevention and management of disability, dressing material, supportive medicines and micro-cellular rubber (MCR) footwear are provided to leprosy patients. The patients are also empowered with trainings in self-care procedure for preventing aggravating disability to the insensitive hands/feets. Emphasis is also being placed on correction of permanent disability through reconstructive surgeries (RCS). To strengthen RCS services, GOI has identified 112 institutions for conducting RCS based on the recommendations of the state governments. Out of these, 60 are Govt. Institutions and 52 are NGO institutions. The patients concerned are provided RCS facility not only free of cost, but are also paid welfare allowances.
- Supervision and Monitoring –Programme is being monitored at different level through analysis of monthly progress reports, through field visits by the supervisory officers and programme review meetings held at central, state and district level. For better epidemiological analysis of the disease situation, emphasis is put on assessment of New Case Detection and Treatment Completion Rate and proportion of grade II disability among new cases. Visits by Joint monitoring Teams with members from GOI, ILEP and WHO have been as integral part of NLEP.
- NGO services under SET scheme- NGOs are getting grants from Govt. of India under Survey, Education and Treatment (SET) scheme. Various activities undertaken by the NGOs are IEC, Prevention of Impairments and Deformities, Case Detection and MDT Delivery. From Financial year 2006 onwards, Grant-in-aid is being disbursed to NGOs through State Health Societies.
Prioritization of the Districts to reduce the leprosy Burden: The World Health Organization (WHO) facilitated an independent evaluation of NLEP from 1 to 14 November 2019. Districts were prioritized based on the leprosy burden. Annual new cases detected, ANCDR, G2D rate, prevalence rate during 2008-2018 were taken into consideration for categorization of the districts.
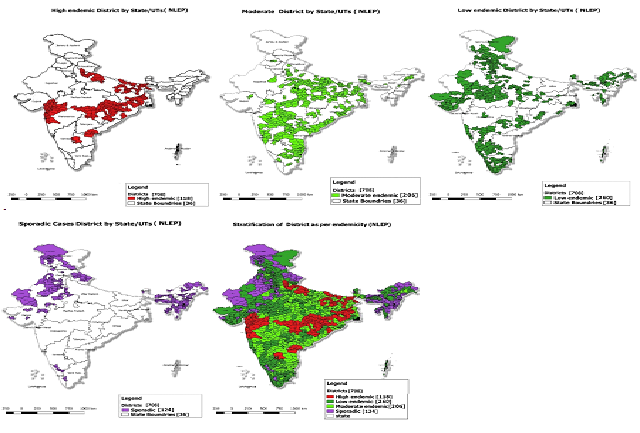
.
Geometric mean for ten years of each of the data element was considered more appropriately representing the situation in the country. Weightages were applied for new case detection, number of new cases with G2D, number of child cases and registered prevalence and used for categorizing districts according to endemicity. The weightages for each of the cases was as follows:
ü Number of the new cases: 40%
ü Registered prevalence: 20%
ü Number of child cases: 20%
ü Number of the new cases with G2D: 20%
Details of endemicity
|
State Of Union Territory
|
Total Districts
|
High endemic districts
|
Moderate endemic districts
|
Low endemic districts
|
Districts with sporadic cases only
|
|
Total Country Number
|
708
|
118
|
206
|
260
|
124
|
|
Total Country %
|
100%
|
17%
|
29%
|
37%
|
17%
|
|
Percentage of country population
|
100%
|
24%
|
39%
|
30%
|
7%
|
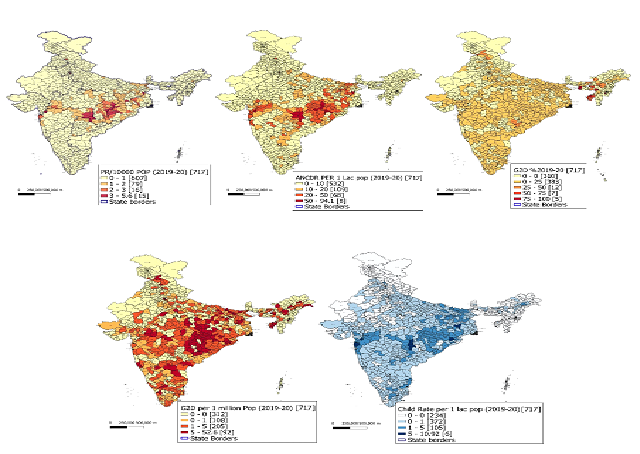
Achievements during 2020:
• Percentage of Grade II Disability (G2D)/visible deformity among new cases decreased from 3.05% in 2018-19 to 2.39% (2019-20).
• The G2D amongst new cases/ million population decreased from 2.65/million population as on 31st March, 2019 to 1.94/million population as on 31st March 2020.
• Child cases percentage has reduced from 7.67% as on 31st March 2019 to 6.86 % as on 31st March 2020.
Epidemiological Indicators of NLEP (2019-20)
NEW INITIATIVES :
1) Enhanced active & early case detection strategy has been introduced through ACD&RS (Active Case Detection and Regular Surveillance strategy throughout the year).
2) Convergence of leprosy screening for targeting different age groups like under RBSK (for 0-18 yrs), RKSK (13-19 yrs), and CPHC – Ayushman Bharat (above 30+ yrs population).
3) Timely referral and follow up for treatment completion on time through Multi Drug Therapy (MDT) available free of cost in all public health facilities
4) For prevention of leprosy amongst contacts: Post Exposure chemoprophylaxis administration (PEP)
5) Awareness Activities: Routine IEC activities are conducted by states and districts throughout the year, Special Annual Mass Awareness campaigns named Sparsh Leprosy Awareness Campaigns (SLAC) were launched on 30th January, 2017 i.e., Anti Leprosy Day, to reduce stigma and discrimination against persons suffering from leprosy. Since then every year, nationwide Gram Sabhas in villages across the country are being organised in cooperation and coordination with allied sectors of health department. Appropriate messages from District Magistrates and appeals from Gram Sabha Pramukh (Heads of Village councils) to reduce discrimination against persons affected with leprosy are read out; pledge is taken by all Gram Sabha members to reduce the burden of disease in the community, and felicitation of persons affected with leprosy is done. Village community is encouraged to participate in these meetings, and school children are encouraged to spread awareness about the disease through plays, posters etc.
.png)
“Sapna” is a concept (mascot) designed and developed using a common girl living in community, who will help spread awareness in thecommunity, through key IEC messages. Sapna can be local school going girl who is willing to be ‘Sapna’.There can be any number of Sapnas in a village.
District award guidelines August,2021  0
0
Active Case Detection and Regular Surveillance for Leprosy(ACD and RS)  0
0
Annual Report April, 2019 to March 2020  0
0
Revised CBAC form  0
0
Screening and Referral tool for children(6-18 years)  0
0
Screening and Referral tool for children(0-6 years)  0
0
Master Issue of NLEP newsletter October 2018-September 2020  0
0
Coffee Table book on " Commemoration of 150th Birth Anniversary of Mahatma Gandhi Ji"  0
0
Sparsh Leprosy Awareness Campaign guidelines for 2019  0
0